Diabetes is a common lifestyle disorder that poses a major health problem to the world. There may be many predisposing factors like an unhealthy diet, sedentary lifestyle, genetic factors, and others. Two types of diabetes are commonly recognized- namely, type 1 that affects the younger population, and type 2 that affects older people. As per WHO estimates, there are about 25 million diabetics in India. Our country is expected to become the diabetes capital of the world by 2025.
The majority of diabetics suffer from a complication called Diabetic Retinopathy. The latter is one of the leading causes of blindness in India. It is a vascular disease of the retina, i.e. which affects the blood vessels. The risk of visual loss is 25 times higher in diabetics than in non-diabetics.
How diabetes affects the eye
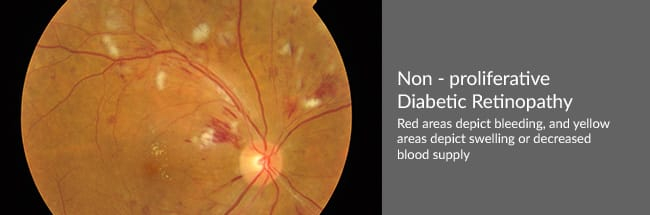
Diabetic Retinopathy affects the blood vessels of the eye. They become weak, particularly, the smaller vessels. Such changes are accompanied by others within the retina, and may contribute to visual deterioration. Retinopathy, broadly, occurs in two stages:
- Non-proliferative retinopathy – changes are less severe than in the proliferative stage. However, decrease in vision may occur as in Macular Oedema.
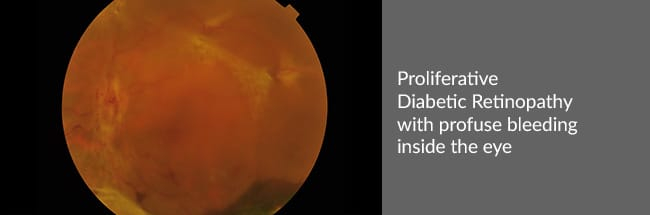
- Proliferative retinopathy – characterized by the development of new blood vessels. They grow, bleed and lead to complications like Retinal Detachment and Neovascular Glaucoma.
Symptoms
Diabetic Retinopathy is a slowly progressive disease of the eye so that patients may not have any symptoms initially. Diminution of vision due to diabetes is only late in the course of the disease so that the condition is often recognized in its advanced stages when intensive control can only minimize its progression but not reverse it. Since only an ophthalmologist can recognize the early signs of Diabetic Retinopathy, it is advised that all diabetics should have their eyes examined at least once a year.
Investigations that maybe required
The patient may require certain ophthalmic tests in case retinopathy is detected.
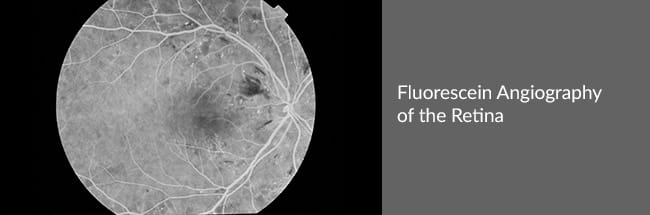
- Fundus Fluorescein Angiography (FFA) – in this test, a photograph of the retina of the eye is taken after injecting a dye into the blood stream. This helps study the vasculature of the retina in greater detail, detect areas of leakage and neovascularization.
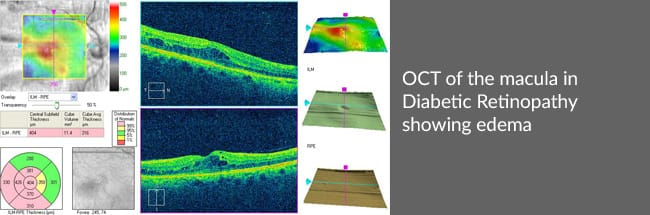
- Optical Coherence Tomography (OCT) – may be required in some diabetics in case macular oedema is suspected. It helps to measure the degree of fluid accumulated and decide an appropriate mode of treatment for it.
Treatment
The treatment for Diabetic Retinopathy depends upon the stage of the disease. In the early stages, control of blood sugar levels helps control the disease and even reverses the changes that have occurred. But later on, Argon Laser Photocoagulation of the retina may be required to control disease progression. Macular Oedema can be sight threatening if treatment is delayed. It requires injection of a steroid inside the eye, or an ‘anti-VEGF’ agent if severe. Proliferation requires laser treatment, even injection of anti-VEGF agents, if extensive. A number of complications may also occur inside the eye in very advanced stages. Of these, Retinal Detachment is quite common. It requires surgical intervention.


