What is Uveitis?
The eye is shaped like a three layered ball. The outermost layer is the sclera, the inner layer is the retina and the middle layer is termed the uvea. Inflammation of this middle layer of the eyeball is called Uveitis.
Causes
In most cases of Uveitis, the underlying cause leading to the condition remains unknown even after detailed laboratory tests. Thus, most cases of Uveitis are termed idiopathic (no underlying cause). The rest of the cases of Uveitis may be associated with various systemic diseases like rheumatoid arthritis, sarcoidosis, inflammatory bowel disease, etc. Some may be due to auto-immunity to ocular antigens while others may occur as a result of infection (viral, bacterial, fungal, parasitic) or trauma.
Types of Uveitis
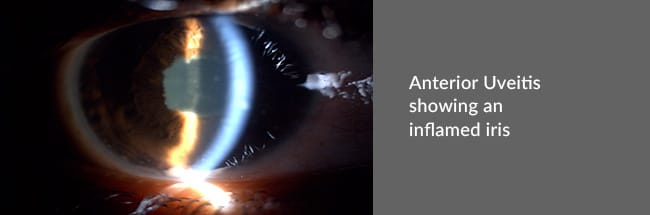
- Anterior Uveitis – The uvea in the front portion of the eye is affected.
- Intermediate Uveitis – The middle portion of the uvea is affected, particularly the muscle that focuses the lens.
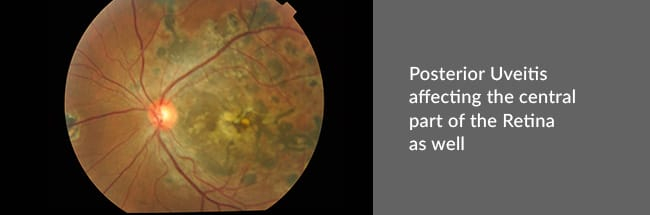
- Posterior Uveitis – Affects the uvea at the back of the eye. The retina may also be affected with posterior Uveitis.
- Panuveitis – Affects the entire uvea, anterior, intermediate, as well as posterior.
Consequences of Uveitis
The uvea is that part of the eye that contains a lot of blood vessels, and thereby, provides nourishment to the tissues of the eye. Uveitis, when untreated, can affect the nourishment and nutrition of the eye, and may even prove to be sight threatening.
Symptoms
Patients may experience one or more of the following.
- Redness of the eyes
- Watering
- Ocular pain
- Glare and intolerance to bright lights
- Decreased vision
- Blurry vision
- Black spots in front of the eyes
Investigations that may be required
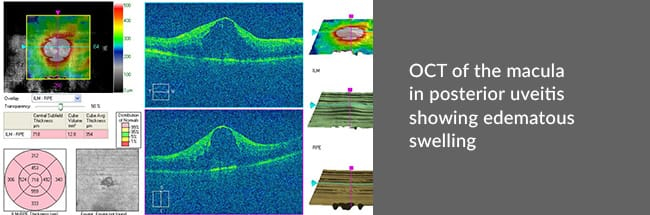
Patients may require a host of blood tests, X-rays, other tests in order to find out the cause of the condition. Some may even require Fundus Photography, Fundus Fluorescein Angiography (FFA) or Optical Coherence Tomography (OCT) for visualization of the posterior part of the eye.
Treatment
Medical treatment suffices for most patients of Uveitis. The aim is to control inflammation. Steroids are given as eye drops or tablets. They may even be injected into or around the eye in some cases. Eye drops to dilate the pupil and relax the ciliary muscle are prescribed. Consequently, patients might experience increased glare and difficulty in near work, but this is merely drug induced. Additional drug therapy may be added, directed to an underlying cause, if found.
When inflammation is severe or unresponsive, immunosuppressive drugs can be resorted to. The latter do have side-effects but are mostly reversible on stoppage of treatment.
Important advice for Uveitis patients
- Use medications as prescribed by the doctor.
- Medications, should preferably, be scheduled and used at a particular time.
- When on steroids, oral or eye-drops, never stop the drug suddenly without consulting the doctor, or the consequences could be very serious.
- In case of any deterioration in symptoms or vision, the doctor should be informed.


